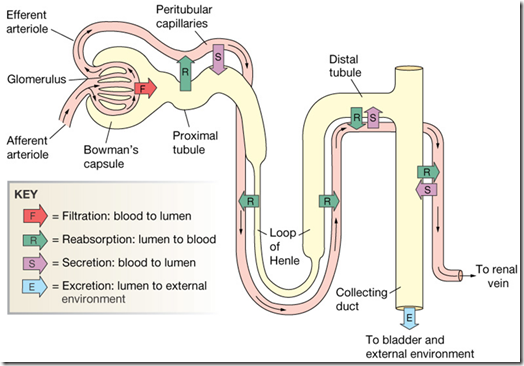
Tubular reabsorption: occurs as filtrate flows through the lumens of proximal tubule, loop of Henle, distal tubule, and collecting ducts.
Following Processes are used in reabsorption:
Diffusion
Facilitated diffusion
Active transport
Co-transport
Osmosis
Reabsorbed substances are transported to interstitial fluid and reabsorbed into peri tubular capillaries.
•The luminal cell membranes are those that face the tubular lumen (“urine” side)
•The basolateral cell membranes are those are in contact with the lateral intercellular spaces and peritubular interstitium (“blood” side)
•The term transcellular refers to movement of solutes and water through cells
•The term paracellular refers to movement of solutes and water between cells
•Epithelial cell junctions can be “leaky” (proximal tubule) or “tight” (distal convoluted tubule, collecting duct)
Types Of Transport Processes:
•Passive transport (simple diffusion)
•Facilitated diffusion
•Primary active transport
•Secondary active transport
•Pinocytosis
•Solvent drag
Passive transport (simple diffusion):
Definition:
•Movement of a substance across a membrane as a result of random molecular motion
Characteristics:
–No metabolic energy required
–Rate of transfer dependent on electrochemical gradient across membrane and membrane permeability characteristics
–Rate of transfer linearly related to concentration of diffusion substance (no Vmax)
Facilitated diffusion: Definition
•Movement of a substance across a membrane down its electrochemical gradient after binding with a specific carrier protein in the membrane
Characteristics:
•The transport protien channels are Saturable (has a Vmax)
•Structural specificity and affinity of carrier for substance transported
•Transfer may occur in either direction across membrane
•Does not directly require metabolic energy
Examples:
•Glucose, amino acids: Basolateral membranes of proximal tubules
•Sodium: luminal membranes of proximal tubules
Primary active transport: Definition
•Movement of a substance across a membrane in combination with a carrier protein but against an electrochemical gradient
Characteristics:
•the transport system is Saturable (has a Vmax)
•Directly requires metabolic energy (i.e. hydrolysis of ATP)
•Structural specificity and affinity of the carrier for
Examples:
•Na+-K+ ATPase
•H+ ATPase
•H+-K+ ATPase
•Ca+2 ATPase
Secondary active transport: Definition
•Two substances interact with one specific carrier in the cell membrane and both substances are translocated across the membrane
–Co-transport: Transported substances move in the same direction across the membrane
–Counter-transport: Transported substances move in opposite directions across the membrane
Characteristics:
•“Uphill” transport of one substance is linked to “downhill” transport of another substance
•Carrier must be occupied by both substances (or be unoccupied) to be mobile in the membrane
•Saturable (has a Vmax)
•Demonstrates specificity and affinity of carrier for substance transported
•“Uphill” transport occurs without direct input of metabolic energy
Examples:
•Glucose, amino acids, or phosphate with sodium in luminal membranes of proximal tubules
•Sodium and hydrogen ions in luminal membranes of proximal tubules
Pinocytosis
•Definition: Uptake by cells of particles too large to diffuse through the cell membrane
•Example: Reabsorption of filtered proteins in the proximal tubules
Solvent Drag:
•A solvent such as water moving across an epithelium by osmosis can drag dissolved solutes with it
Glucose and Aminoacids Reabsorption:
•Filtered glucose & amino acids are normally 100% reabsorbed from filtrate
–Occurs in PCT (proximal convoluted tubules) by carrier-mediated cotransport with Na+
•Transporter displays saturation if ligand concentration in filtrate is too high
–Level needed to saturate carriers & achieve maximum transport rate is transport maximum (Tm)
–Glucose & amino acid transporters don't saturate under normal conditions
Significance of PCT Reabsorption:
•≈65% Na+, Cl-, & H20 is reabsorbed in PCT & returned to bloodstream
•An additional 20% is reabsorbed in descending limb of the loop of Henle
•Thus 85% of filtered H20 & salt are reabsorbed early in tubule
–This is constant & independent of hydration levels
–Energy cost is 6% of calories consumed at rest
–The remaining 15% is reabsorbed variably, depending on level of hydration
Loop Of Henle
Descending Limb:
•Is permeable to H20
•Is impermeable to salt
•Because deep regions of medulla are 1400
mOsm, H20 diffuses out of filtrate until it equilibrates with interstitial fluid
–This H20 is reabsorbed by capillaries
Ascending Limb:
•Has a thin segment in depths of medulla & thick part toward cortex
•Impermeable to H20
•Permeable to salt
•Thick part ATs salt out of filtrate
–AT of salt causes filtrate to become dilute (100
mOsm) by end of LH
Active transport in ascending limb:
•NaCl is actively extruded from thick ascending limb into interstitial fluid
•Na+ diffuses into tubular cell with secondary active transport of K+ and Cl-
Counter Current Multiplier:
•Countercurrent flow & proximity allow descending & ascending limbs of LH to interact in way that causes osmolarity to build in medulla
•Salt pumping in thick ascending part raises osmolarity around descending limb, causing more H20 to diffuse out of filtrate
–This raises osmolarity of filtrate in descending limb which causes more concentrated filtrate to be delivered to ascending limb
–As this concentrated filtrate is subjected to Active transport of salts, it causes even higher osmolarity around descending limb (positive feedback)
–Process repeats until equilibrium is reached when osmolarity of medulla is 1400
Vasa Recta:
•Is important component of countercurrent multiplier
•Permeable to salt, H20 (via aquaporins), & urea
•Recirculates salt, trapping some in medulla interstitial fluid
•Reabsorbs H20 coming out of descending limb
•Descending section has urea transporters
•Ascending section has fenestrated capillaries
Collecting Ducts:
•Plays important role in water conservation
•Is impermeable to salt in medulla
•Permeability to H20 depends on levels of ADH
ADH ( Anti Diuretic Hormone )
•Is secreted by posterior pituitary in response to dehydration
•Stimulates insertion of aquaporins (water channels) into plasma membrane of CD
•When ADH is high, H20 is drawn out of CD by high osmolality of interstitial fluid
–& reabsorbed by vasa recta
Formation Of Concentrated Urine:
•ADH-dependent water reabsorption is called facultative water reabsorption
•ADH is the signal to produce concentrated urine
•ADH stimulates formation of aquaporins in membrane of tubule cells. Increases water reabsorption from filtrate
•The kidneys’ ability to respond depends upon the high medullary osmotic gradient



Comments
Post a Comment
Post Your Reply and Give Your Opinion About the Post